Introduction
A posterior chamber phakic intraocular lens is an important consideration in refractive surgery. This type of lens is inserted into the eye that has an intact natural crystalline lens to enhance uncorrected vision. The implantable collamer lens (ICL) is currently the only approved posterior chamber phakic lens in North America. Most eye surgeons and practices refer to this lens as the implantable contact lens. It is a soft, thin lens that can be surgically implanted to correct nearsightedness, farsightedness, and astigmatism, as shown in Figure 1.1–3 This lens offers a long-term alternative to traditional contact lenses.
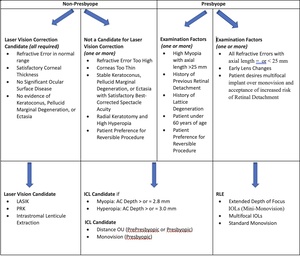
A posterior chamber phakic lens is inserted into the space between the iris and the crystalline lens and is a reversible option for refractive surgery (Figure 2). Other options include LASIK, PRK, Intrastromal Lenticule Extraction, and Refractive Lens Exchange, but unlike these procedures, the phakic lens does not require tissue removal. It is rare for patients to have a phakic implant extracted except at the time of cataract surgery. A comparison of the benefits and risks of the most common refractive procedures is provided in Table 1.
Patients who are candidates for a phakic implant should receive counseling on the ICL procedure and be provided with a comparison of ICLs, laser vision correction, and RLE to make an informed decision (Table 2). Clinicians should have a comprehensive understanding of the procedure’s indications, contraindications, surgical technique, and postoperative complications to provide adequate pre- and postoperative care.
The EVO Implantable Collamer Lens
Globally, over two million ICLs have been implanted, and it has been approved for clinical use in Canada for over 20 years.4 The innovative EVO ICL design with a central microscopic opening of 0.36 mm in the optic is available for myopic eyes since approval in Canada in 2016. This design enhances fluid dynamics around the crystalline lens, improves aqueous circulation, and reduces the risk of pupillary block glaucoma.1 The fluid flow has resulted in improved hydration of the crystalline lens and a resultant low incidence of cataract formation with long-term data from Europe.5 Additionally, the central port eliminates the need for peripheral laser iridotomies, which makes the entire surgical process easier for patients.
Unlike typical intraocular lenses that are stored on the shelves in eye operating rooms, the ICL is custom ordered and manufactured according to the refractive error and ideal length of the lens. The lens’s length determines the vault over the crystalline lens, with the aim of achieving satisfactory clearance while avoiding excessive vault that could lead to a shallow anterior chamber.
Based on a review of 67 preclinical studies and clinical reports, which evaluated 1,905 eyes with an average follow-up period of 12.5 months for effectiveness and 4,196 eyes with a weighted average follow-up period of 14.0 months for safety, the EVO ICL has been deemed both safe and effective in treating a wide range of refractive errors.1 The EVO ICL has demonstrated its effectiveness through high levels of postoperative uncorrected visual acuity, refractive predictability, and stability. Moreover, the safety data indicate lower rates of anterior subcapsular cataract and pupillary block as compared to earlier models.1 These improvements in safety and efficacy make the EVO ICL a desirable choice for both patients and surgeons.
Patients have reported significant improvements in quality of vision and quality of life using the Quality of Life Impact Refractive Correction questionnaire.6 In a peer-reviewed comparison of optical quality and intraocular light scattering, the EVO lens with a central port did not significantly affect the lens’s optical performance compared to older ICLs without the central port.7
Unlike corneal refractive surgical procedures, the ICL implantation does not alter the cornea’s shape, so the selection of IOL power for future cataract surgery is not affected. Keeping the cornea intact also eliminates the potential for a dry eye.1
In a study of 351 eyes, the postoperative uncorrected visual acuity of the EVO ICL group was 20/20 or better in 97%, 100%, 100%, 100%, 100%, and 85% of eyes at 1, 3, and 6 months and 1, 3, and 5 years after the surgery, respectively.8 This indicates that the postoperative uncorrected visual acuity was excellent and stable for up to 5 years after the surgery.8 Furthermore, the reports also suggest high accuracy and refractive predictability.
EVO ICLs are made of Collamer, a biocompatible material containing collagen bonded with a UV-absorbing chromophore into a poly-HEMA based copolymer, offering UV protection and minimizing inflammation.9
What are the Indications for ICL Surgery?
ICLs are typically recommended for patients who have moderate to severe refractive errors that cannot be effectively corrected by other methods such as laser vision correction or are deemed at high risk of retinal complications with a RLE. The following are the anatomic, refractive, and patient specific indications for the use of ICLs:
Anatomic
-
Myopic ICL: Anterior chamber depth > or = 2.8 mm
-
Hyperopic ICL: Anterior chamber depth > or = 3.0 mm
Refractive Error
-
Myopia -3 to -18 D
-
Hyperopia +3 to + 10 D
-
Astigmatism +1.00 to +6.0 D
It is important to understand that if there is a residual refractive error, then laser vision correction can be performed to optimize uncorrected vision.
Patient Considerations
-
High myopia: ICLs are a good option for patients with moderate to high myopia, who cannot be treated with laser vision correction.10–12 Unlike with laser vision correction, the ICL does not cause flattening of the cornea and therefore reduces the risk of induced spherical aberration, a higher-order aberration that can potentially make driving at night more difficult. For highly myopic presbyopic patients, the ICL is a safer option than RLE because of a reduced risk of retinal detachment and maintaining levels of accommodation by not removing the crystalline lens. Monovision is an option to aid in reading.
-
High hyperopia: Although a high percentage of hyperopes will not qualify for the ICL because of an anterior chamber depth of < 3.0 mm, this is a good option in the pre-presbyopic patient.13,14 Presbyopic patients usually prefer improvement in distance and near and are often satisfactory candidates for RLE. Since the hyperopes usually have shorter axial lengths compared to high myopes, there is a lower risk of retinal tears and retinal detachment.
-
Keratoconus: Patients with stable keratoconus and a satisfactory best-corrected acuity of 20/30 or better, may benefit from ICL surgery.15–17 For patients less than 35 years of age, corneal crosslinking is usually recommended to stabilize the corneas, and then to wait approximately 12 months for refractive stability prior to ICL surgery. Older patients with topographic and refractive stability do not require corneal crosslinking prior to ICL surgery. In patients with reduced best-corrected acuity, a topographic-PRK (TG-PRK) ablation and crosslinking may be indicated (Figure 3). TG-PRK is an excimer laser ablation of the cornea that is guided by topography to reduce irregular astigmatism by flattening steep areas and steepening flat areas. If best-corrected acuity is satisfactory, then an ICL could be performed.
-
Radial keratotomy: Patients may be overcorrected because of excess flattening from the radial incisions.18 Although they can have success with a RLE, the IOL calculations are less accurate following radial keratotomy, and in addition there is a greater risk of retinal tears and retinal detachment because of the longer axial length in the myopic eye.
-
Piggyback lens: Patients that have had cataract surgery or refractive lens exchange can be treated with an ICL inserted in the ciliary sulcus in front of the initial implant.19 This can result in a quick improvement in uncorrected acuity.
-
Thin corneas: Some patients may have corneas that are too thin to undergo laser vision correction. ICL can be a good alternative in these cases. Patients that have had laser vision correction and have regressed with thin corneas may be satisfactory candidates for an ICL as an enhancement. In this situation patients may have any degree of refractive error.
-
Dry eye syndrome: Traditional contact lenses can be uncomfortable for people with dry eye syndrome. In this situation, laser vision correction may be contraindicated as the surface curvature changes may aggravate a dry eye.
-
Desire for improved visual acuity: Implantable contact lenses can provide sharper and clearer vision than traditional contact lenses or glasses, which can be appealing for people who value their visual acuity. When the vision is corrected closer to the nodal point of the eye, vision is typically better than with optical aids.
What are the contraindications for the ICL?
While ICLs can be a safe and effective option for many patients with refractive errors, there are certain contraindications that may make some individuals unsuitable candidates for the procedure.20 These may include:
-
Age: Implantable contact lenses are generally not recommended for individuals under the age of 21, as their refractive error may still be changing.
-
Pregnancy or breastfeeding: Hormonal changes during pregnancy and breastfeeding can affect the refractive error, which can make it difficult to determine the proper ICL prescription.
-
Unstable refraction: Individuals whose vision prescription has changed significantly within the past year may not be good candidates for ICL surgery.
-
Primary Open Angle or Narrow Angle Glaucoma.
-
Patients with Fuchs’ Dystrophy or a low endothelial cell count.
-
Visually significant Cataracts.
-
Patients who have significant Amblyopic or Blind in the fellow eye.
-
Anterior chamber depth (as measured from the corneal endothelium to the anterior lens capsule) of < 2.8 mm for myopic eyes, and < 3.0 mm for hyperopic eyes.
Surgical Procedure
The ICL procedure is performed under topical anesthesia without the need for injections or sutures. Patients are usually given a mild sedative to make them more relaxed. In the operating room, if a toric implant is to be inserted the axis for the implant is marked on the cornea with the patient sitting up. The patient is then positioned in a supine position on the operating room bed, and the periorbital area and eye is cleaned with a disinfectant solution like Betadine. A surgical drape is applied to keep the operating field sterile. A 1 mm incision and 3 mm incision are made in the peripheral cornea in the limbus area. The smaller incision is used for injection of an intracameral anesthetic, a viscoelastic to maintain space in the anterior chamber and protect the crystalline lens, and for a thin instrument to position the haptics behind the iris and position the ICL in the correct orientation. The larger incision is used to insert the ICL through an injector system. Through the injector, the folded lens opens slowly in the anterior chamber and then the haptics are tucked behind the iris so the lens is positioned in the posterior chamber in front of the crystalline lens. The wounds are hydrated to decrease leakage, and no sutures are required. An antibiotic is injected to decrease the risk of infection. Patients are given an antibiotic, steroid, and nonsteroidal drops to be used postop for a few weeks.
Postoperative Care
Patient follow-up is typically at one day, one to two weeks, and then one month. The examination includes measuring uncorrected acuity, best-corrected acuity, intraocular pressure, and slitlamp examination. The pupils should be equal in size, there should be a satisfactory vault of the ICL over the crystalline lens, and the anterior chamber should not be shallow.
What are the potential postoperative complications?
The surgeon and the surgical team are primarily responsible for discussion of the benefits, and risks including potential complications of a posterior chamber phakic implant. The phakic lens is generally considered safe and effective for correcting vision problems and have a low risk of complications. However, as with any surgical procedure, there is a small risk of complications.
Regular follow-up appointments with an eye doctor can help to monitor for any potential complications and ensure the best possible outcome.
-
Elevated intraocular pressure: In the first 24 hours, there is a risk of elevated intraocular pressure because of the viscoelastic trapped behind the ICL.21 Patients may complain of headache, nausea, or vomiting. The use of a pressure lowering drop, an oral agent like Diamox, can be helpful. Prior to the development of the EVO ICL for myopia, and currently with the hyperopic ICL that doesn’t have a central opening, pupillary block glaucoma could occur.22 In this situation, a YAG iridotomy needs to be repeated, and this is usually successful in lowering the eye pressure. In rare situations, the ICL can be too large resulting in a significant vault and shallow anterior chamber.23 In this situation, the pressure is very difficult to control, and the ICL may need to be removed. If the elevated pressure is seen only after a week and the anterior chamber has a satisfactory depth, then this is usually a reaction to the steroid drops. Discontinuing the steroid usually results in the pressure returning to normal within a week.
-
ICL touching the crystalline lens: This is related to a sizing issue with the ICL with the lens being too short. This is extremely rare and may require removal of the lens with replacement of a larger ICL.
-
Infection: As with any intraocular surgical procedure, infection is a very rare complication and associated with a decrease in vision, redness of the eye, and a significant anterior chamber reaction often with a hypopyon.24 Infections in the eye can be serious and can lead to vision loss if not treated promptly.
-
Vitreous floaters: A vitreous detachment often results in the onset of floaters. These can be bothersome but, in most patients, decrease over time.
-
Retinal tear/Retinal Detachment: A vitreous detachment can lead to a retinal tear and the potential of a retinal detachment.25 A study conducted a retrospective chart review to evaluate the risk of retinal detachment (RD) following implantable collamer lens (ICL) implantation in myopic eyes. The study, which spanned a period of 10 years, concluded that ICL implantation did not increase the risk of RD compared to myopic eyes that were not operated on.26 Previous research has suggested that the incidence of pseudophakic RD is higher in eyes with certain risk factors such as longer axial length (>25 mm), a history of lattice degeneration or ocular trauma, a previous history of RD in the other eye, younger age (< 60 years), male gender, and intraoperative complications like posterior capsular rupture. In myopic eyes (>25 mm), there is a six-fold increased risk of pseudophakic RD, and this risk is further amplified by another six-fold in younger myopic patients (<60 years).27 To provide context, individuals younger than 60 years who are myopic and undergo lens-based surgery have a 12-fold increased risk of pseudophakic RD.27
-
Glare or halos: If the ICL optic is not well centered around the pupil then patients can have symptoms that my not improve.28 In this situation, repositioning the lens can be helpful. In the case of the EVO ICL there may be light scatter from the central opening.29 Patients may experience some glare and halos, but this typically decreases secondary to a brain mechanism called neuroadaptation. The brain sees some unwanted images and simply suppresses these over time resolving the symptoms.
-
Residual refractive error: The accuracy of the refractive correction is very accurate with the ICL as there is essentially no significant healing that takes place compared to laser vision correction with epithelial remodelling of the cornea. In addition, regression is rare compared to laser vision in high prescriptions. If a residual refractive error does occur, rather than exchanging the ICL, the safest option is laser vision correction to refine the vision.
-
Corneal endothelial cell loss: During ICL surgery, there is a risk of loss to the cells that line the back of the cornea.30,31 Based on the clinical data collected through 5-7 years postoperative, the calculated rate of loss of endothelial cell density (ECD) was 1.8% per year. This means that on average, a patient who has undergone ICL implantation can expect to lose approximately 1.8% of their endothelial cells each year following the procedure.32 It’s important to note that this rate of loss should be viewed in the context of the expected age-related loss of ECD, which is 0.6% per year.33 This means that even though the rate of loss is higher than what is typically seen with aging alone, it is still within the range of what is considered normal. Furthermore, the fact that no cases of corneal decompensation in the absence of trauma have been reported following ICL implantation is a positive sign for the long-term health of the corneal endothelium after this procedure. It suggests that even with the higher rate of cell loss, the remaining cells are able to compensate sufficiently to maintain corneal health and prevent decompensation.
-
Cataracts: ICL surgery may increase the risk of developing cataracts later in life, however with the development of the EVO ICL, with the central port, has decreased the risk.34 Safety data indicate that EVO lenses may reduce the occurrence of anterior subcapsular cataract (ASC) compared to earlier ICL models. A review of 38 peer-reviewed papers with safety data from retrospective and prospective studies on the EVO ICL, including 4196 eyes with up to 5 years of follow-up, showed that no patient developed a visually significant ASC, and only one eye experienced pupillary block due to retained viscoelastic.35 It is important to recognize that high myopic patients often develop cataracts earlier in life. Cataract surgery can be very successful with the removal of the ICL and cataract, and with the insertion of a new intraocular lens.
-
Dislocation: In rare cases, the ICL may shift out of position usually secondary to trauma.36,37 Surgical repositioning can restore the vision.
Summary and Clinical Experience
A posterior chamber phakic implant is a highly effective option for patients seeking long-term refractive stability and safety, leading to improved uncorrected acuity. Although it is commonly used for high myopia, it can also be a viable option for patients with thin corneas, keratoconus, radial keratotomy, pre-presbyopic hyperopes, and as a piggyback lens following cataract surgery and RLE. The refractive accuracy is comparable to that of fitting a contact lens on the cornea, and complications are minimal, resulting in a high benefit-to-risk ratio for patients. Patients also experience a high level of satisfaction due to the quick improvement in uncorrected acuity.
Additionally, by preserving the natural corneal curvature, the quality of vision is excellent both during the day and at night. It is essential for clinicians to be knowledgeable about this innovative procedure so as to offer the best options to their refractive surgery patients and improve their quality of life.
_with_a_central_opening_in_the_optic_that_is_insert.png)



_with_a_central_opening_in_the_optic_that_is_insert.png)



