Introduction
Posterior capsular opacification (PCO) due to lens epithelial cell growth from the remaining lens capsule occurs in up to 19% of eyes three years after cataract surgery with a posterior chamber intraocular lens (PCIOL).1,2
In some cases, however, the PCIOL itself can become opacified, a condition known as lens glistening. It is important to distinguish between PCO and glistening as the management of the two conditions differs: symptomatic patients with PCO are treated with YAG laser; patients with lens glistening are managed with observation or require an intraocular lens exchange depending on symptoms and the view of the fundus. A recent review of intraocular lens (IOL) opacifications reported glistening affects vision from induced glare rather than a reduction of acuity or contrast sensitivity.3 The incidence of glistening varies depending on the material of the IOL with 66-100% incidence rates for older hydrophobic acrylic lenses.3 We herein present a patient with symptomatic lens glistening without a reduction in visual acuity.
Case Presentation
An 86-year-old Caucasian male presented with complaints of moderate increased blur in the left eye for the past four months that did not affect his activities of daily living (ADLs). His ocular history was remarkable for cataract surgery in both eyes eight years prior to presentation, acute angle closure treated with laser peripheral iridotomy, macular retinoschisis, and vitreoretinal traction – all in both eyes. In addition, he had senile peripheral retinoschisis of the right eye. Significant past medical history included chronic arthritis, hyperlipidemia, hypertension, asthma, and peripheral artery occlusive disease. Significant systemic medications included hydroxychloroquine (for three years), atorvastatin, lisinopril, metoprolol, and albuterol inhalant.
On examination, best-corrected visual acuity was 20/20 in the right eye and 20/20 in the left eye. Pupils, extraocular motilities, and confrontation visual fields were all unremarkable.
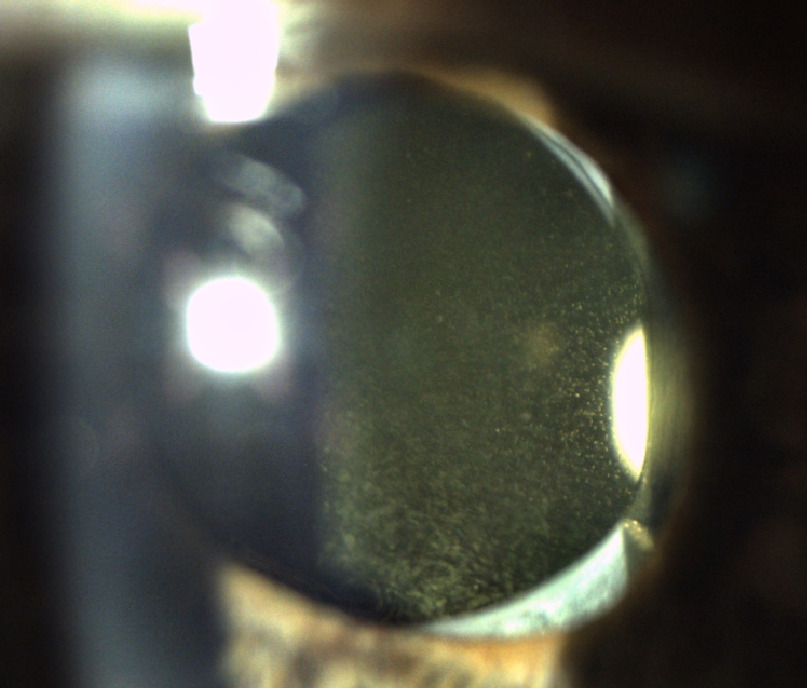
The anterior segment was remarkable for patent laser peripheral iridotomies and PCIOL opacities in both eyes. The opacities reflected light and had a glistening appearance, greater in the left eye than the right eye (Figure 1). Dilated fundus examination was notable for shallow temporal and inferior peripheral retinoschisis of the right eye and a flat choroidal nevus inferonasal in the left eye three-quarters of a disc diameter in size.
Optical coherence tomography (OCT) showed separation of inner and outer retinal layers inferior to the fovea consistent with macular retinoschisis in both eyes with greater separation in the right eye as well as bilateral traction on the nerve fiber layer superior to the fovea consistent with vitreomacular traction. The findings were stable from 2020. There was no evidence of hydroxychloroquine retinopathy on OCT or Humphrey 10-2 visual field testing. Given his stable visual acuity and retinal findings, it was felt that the most likely cause of the patient’s visual disturbance was IOL glistening. The patient was referred to his cataract surgeon for a discussion of observation versus intraocular lens exchange. The decision was made to observe the lens glistening.
Discussion
Lens glistening is a result of fluid filled microvacuoles that can coalesce and grow within the IOL.1 This process occurs due to the salinity of surrounding aqueous and can cause an increase of light scatter.1 The patient can experience visual disturbances such as increase blur or decrease in contrast sensitivity.1
Posterior chamber IOLs vary in their composition. The most common PCIOLs are: collamer, hydrophobic acrylic, hydrophilic acrylic, PEG-PEA/HEMA/Styrene (PHS) copolymer, polymethylmethacrylate (PMMA), and silicone.4 Table 1 describes the pros and cons of these materials as they are used in the eye. Silicone and acrylic IOL are foldable and therefore more useful in small incision surgeries while PMMA are excellent for their rigidity and are used for scleral sutured IOLs in complicated cases.4 Hydrophobic lenses are more likely to result in glistening whereas hydrophilic lenses are more likely to result in PCO.4
One formulation of note is the hydrophobic acrylic compound seen in the following lenses: AcrySof® (Alcon, Fort Worth, Texas, USA), TECNIS® (Johnson and Johnson Vision, Jacksonville, Florida, USA), EnVista® (Bausch and Lomb, Bridgewater, New Jersey, USA), and Vivinex® (Hoya Surgical Optics, Chino Hills, California, USA).1 This common IOL material has the increased potential to develop microvacuoles after implantation due to the salinity of the surrounding aqueous humor.1 The copolymers of the lens allows water to enter and it can create various pockets of lower polymer density which can enlarge to become vacuoles within the IOL.1 This hydrophobic acrylic compound is used due to its ability to be folded and for its lower rates of dense PCO.4 However, implants with this composition have up to a 55% incidence of glistening at one year postoperatively; most patients are asymptomatic.5
Glistening IOLs can be differentiated from PCO based on clinical features. In PCO, the IOL opacities are on the inner surface of the posterior capsule. In IOL glistening, the opacities appear within the implant itself. Depending on the severity, PCO or lens glistening opacities can affect a patient’s ADLs or limit examination of the retina.
Glistening can be objectively graded with anterior segment OCT. The central area of the lens is evaluated under dilated conditions and the microvacuoles are quantified.6 The grading system ranges from grade 0 (“no glistening”), which correlated to less than or equal to 5 microvacuoles, up to grade 3 (“severe glistening”), which correlates to greater than 30 microvacuoles.6 Visual field testing also can be used as an indicator for decreased visual performance using the mean deviation index.3,7
While patients with significant PCO can be treated with a laser posterior capsulotomy, those with glistening IOLs require a lens exchange.8 The patient’s existing IOL is removed surgically and a new IOL is implanted in its place.9 IOL exchange may require complex intra-operative techniques with additional risks of complications.10 Reported complications of lens explantation include zonular dehiscence, posterior capsule rupture, and corneal decompensation.10
The patient in this case had excellent visual acuity with stable underlying retinal disease. The patient’s symptoms were felt to arise from the lens glistening given the stability of his clinical examination, diagnostic imaging, and visual field testing. The patient was managed conservatively.
Disclosure
There are no financial or personal interests to disclose.
Disclaimer
The views expressed in this article are of those of the authors and do not necessarily reflect the position or policy of the United States (US) Department of Veterans Affairs or the US government.