The introduction of Corneal Crosslinking (CXL) in countries worldwide has led to a reduction in the need for corneal transplants in patients with keratoconus.1,2 This innovative and revolutionary procedure is relatively simple in concept, easy for patients to undergo, and can provide excellent outcomes in preserving and stabilizing vision.3–5 By stiffening the collagen fibers of the cornea, CXL can prevent progressive disease and vision loss.6 It is imperative for all eye care professionals to understand the positive long-term impact of this procedure and how it has become the standard of care in the management of selected keratoconus patients and those with other ectatic diseases.
Keratoconus is a condition where the cornea gradually becomes thinner and steeper, causing myopia, astigmatism, and potentially leading to scarring. The pathophysiology of keratoconus is influenced by various factors, including genetic and environmental factors, as well as conditions such as excessive eye rubbing, systemic diseases, allergies, eczema, and floppy eyelid syndrome. If untreated, more than 20% of patients may require a corneal transplant.4 Fortunately, with timely intervention, visual impairment can be avoided, and early treatment can improve the patient’s quality of life while reducing the risk of needing a transplant.
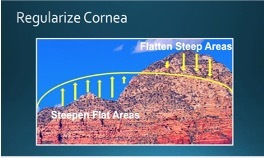
The combination of CXL with topography-guided TG-PRK has been shown to reduce irregular astigmatism and improve best-corrected spectacle acuity.7,8 TG-PRK involves selectively removing tissue to flatten steep areas of the cornea and steepen flat areas
CXL + TG-PRK is most commonly used in the surgical management of keratoconus, pellucid marginal degeneration, and ectasia after laser vision correction (Figure 2). CXL involves applying a photosensitizing agent to the cornea, which is then activated with ultraviolet light. This causes chemical bonds to form between the collagen fibers in the cornea, increasing their strength and stiffness. This paper aims to provide a comprehensive review of the CXL + TG-PRK procedure, including its indications, contraindications, and potential complications.
The Procedure: TG-PRK + CXL
The procedure involves the use of an excimer laser capable of tissue ablation guided by corneal topography, Riboflavin (vitamin B2) drops to penetrate and concentrate in the corneal stroma, and an ultraviolet-A light source. To guide the excimer laser, at least eight preoperative topographic maps are taken and then averaged. The resulting topography data is digitally transferred to the excimer laser and a custom treatment is designed (Figure 3). A Phototherapeutic Keratectomy (PTK) is used to remove the corneal epithelium of approximately 9 mm, which exposes Bowman’s layer. Riboflavin drops are then applied for 10 to 20 minutes, allowing for satisfactory diffusion into the stroma. The specialized ultraviolet-A light source with a wavelength of 370 nm is applied for a specific duration, which causes crosslinking of the corneal collagen fibers, increasing corneal rigidity. To promote healing and comfort, a bandage soft contact lens is applied, and the patient is given antibiotic, steroid, and nonsteroidal drops. The corneal epithelium is typically intact by day 5 postoperatively, at which point the contact lens is removed.
Diagnosis of Keratoconus
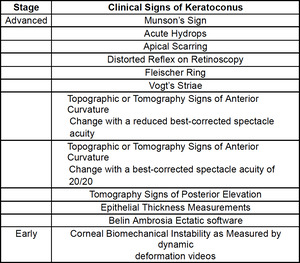
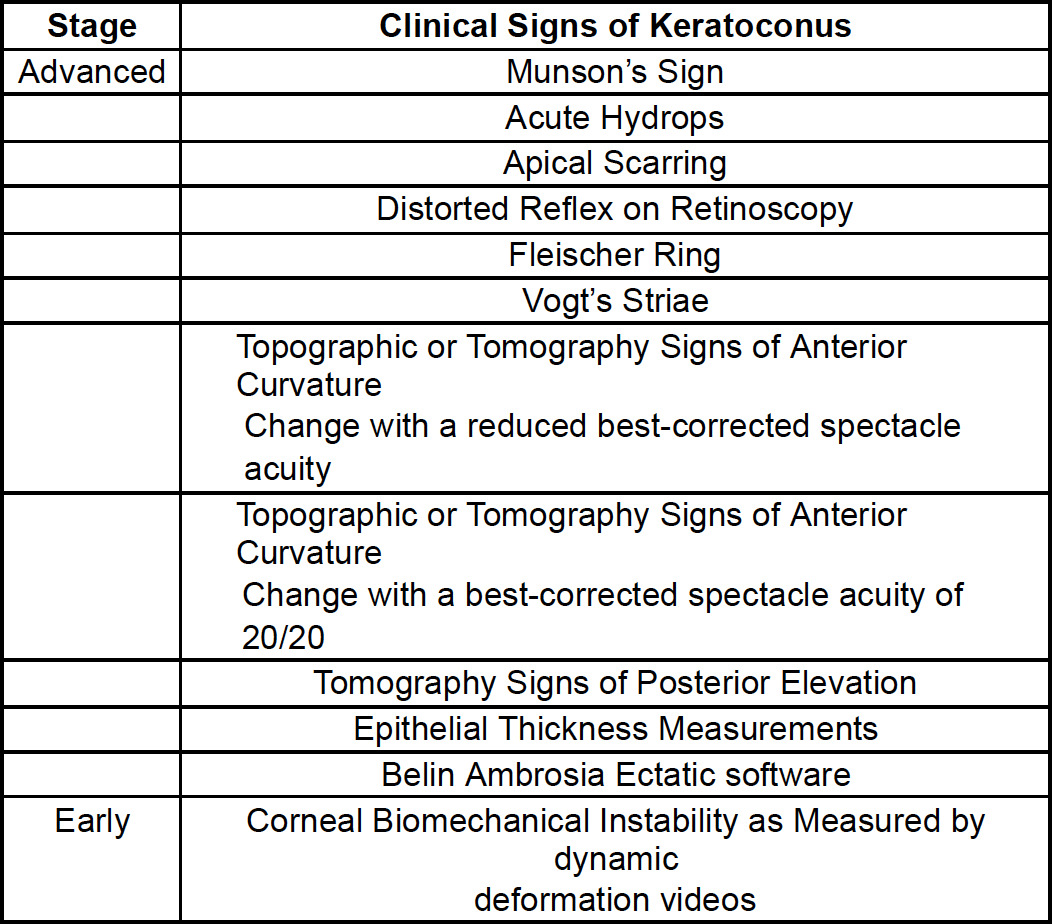
The incidence of keratoconus in the population has increased over time as diagnostic equipment has improved. Table 1 outlines various clinical signs of keratoconus that can be categorized according to whether they occur early or late in the progression of the disease.
Corneal imaging has become the standard diagnostic tool in keratoconus. The following are some findings suggestive of keratoconus,
-
Corneal thinning: The cornea thins and bulges outwards in keratoconus, leading to changes in corneal thickness across different regions. Usually, the thinnest area is in the region of the steepest part of the cornea.
-
Irregular corneal shape: The cornea takes on a cone-like shape in keratoconus, which can be seen as an irregular curvature pattern on the corneal map.
-
Corneal steepening: The curvature of the cornea becomes steeper in the central or paracentral region in keratoconus. This is usually associated with the inferior cornea being 1.4 D steeper than the superior cornea or a central bow- tie pattern9–11 (Figure 4).
-
Corneal asymmetry: The cornea becomes asymmetric, which can be seen as an irregular pattern of curvature on the corneal map.
These findings, when seen together, can provide strong evidence for the diagnosis of keratoconus.
While corneal topographic units are a less expensive option and can provide valuable information, tomography units offer more comprehensive data. They can capture data of both the anterior and posterior corneal surfaces, measure corneal thickness, and utilize artificial intelligence software to determine the probability of ectatic disease. The Belin Ambrosia Ectatic software is the most advanced tool for detecting subtle forms of keratoconus.12 The prevalence of keratoconus using the advanced methods of corneal tomography with the Belin Ambrosia software is 1.2%.13 This is significantly higher than what was detected with topography alone.
Advanced keratoconus can be detected through a slit-lamp examination and may have any of the following findings: stria, apical scarring, and scarring from a previous rupture of Descemet’s membrane. However, early diagnosis is crucial to prevent the progression of the disease, as it can progress rapidly.14 The earlier the diagnosis, the greater the chance of preserving vision. The best time to diagnose keratoconus is when patients have inferior steepening that has not progressed into the pupillary zone and a best corrected acuity of 20/20.
It is important to rule out pseudo-keratoconus, which refers to conditions that can be mistaken for keratoconus but do not require corneal cross-linking .15 This can be done through a slit-lamp examination and corneal imaging. Pseudo-keratoconus conditions include punctate kerotopathy, epithelial basement membrane disease (Figure 5),corneal scar, Salzmann’s nodular degeneration (Figure 6), corneal warpage from hard contact lenses, a poorly captured topographic map (Figure 7), and previous hyperopic laser vision correction (Figure 8).
Indications
Patients diagnosed with progressive keratoconus, as indicated by changes in corneal topography, will require corneal collagen cross-linking (CXL), regardless of their age. However, it is highly recommended that patients under the age of 35 years old, upon diagnosis of keratoconus, should seriously consider CXL due to the high likelihood of disease progression.
CXL has a low risk-to-benefit ratio and has shown to be highly successful in preventing vision loss. The optimal age for treatment depends on the patient’s ability to cooperate during the procedure. Based on our experience, patients as young as Nine years old can undergo CXL treatment.
For patients who undergo TG-PRK + CXL, it is important that their corneal thickness is at least 430 microns. Typically, during TG-PRK, less than 50 microns of stromal tissue is removed. In cases where the corneal thickness is less than 400 microns after epithelial removal and TG-PRK, Riboflavin solutions that induce stromal swelling can be used. This swelling effect can increase the corneal thickness to above 400 microns prior to CXL, ensuring the safety of the corneal endothelium. There are various Riboflavin solutions available that can achieve this outcome.
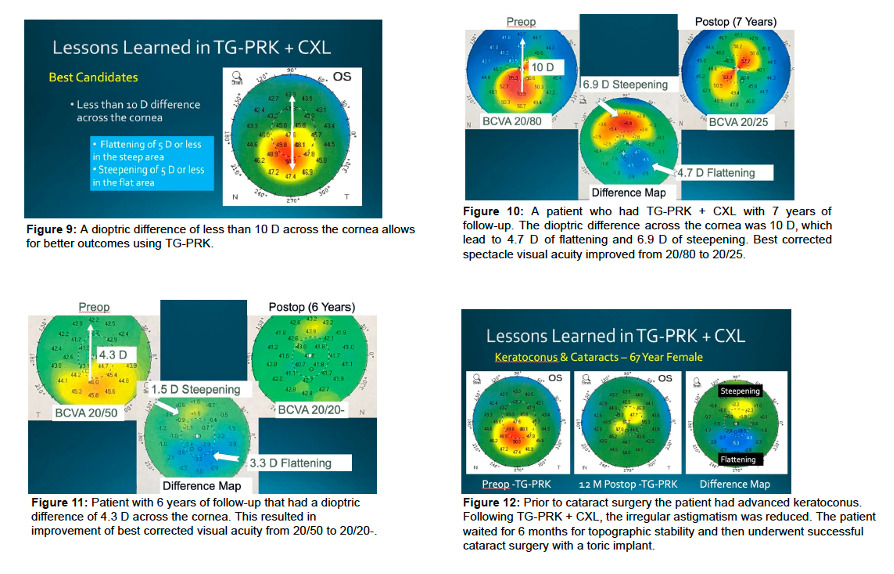
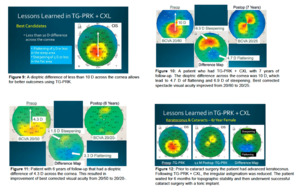
The ideal candidates for TG-PRK + CXL have a dioptric difference of less than 10 D7 across their cornea, which is calculated within a 6 mm optical zone by measuring the difference between the flattest and steepest areas (Figure 9). If the dioptric difference is 10 D, the flat portion of the cornea will be steepened by 5 D, and the steepest portion
will be flattened by 5 D (Figure 10). This represents the upper limit of the technology. However, the very best outcomes are achieved with smaller differences, such as a 5 D difference, where the flat area of the cornea is steepened by 2.5 D, and the steep area is flattened by 2.5 D (Figure 11). When less tissue is removed, the outcomes are more accurate, and there is a lower chance of any induced corneal haze.
TG-PRK + CXL is typically performed on patients with progressive keratoconus or young age with a high probability of progression. There are other situations where the procedure can be utilized, for instance, if a patient has a stable cornea but is intolerant to rigid-gas permeable or scleral contact lenses, TG-PRK + CXL can be offered to reduce irregular astigmatism and decrease dependency on contacts.
Another situation where the procedure can be considered is prior to cataract surgery, as it can reduce the need for hard lenses after implant surgery (Figure 12). However, prior to performing TG- PRK, patients need to discontinue their hard contact lenses for one month or longer to ensure topographic stability.
Contraindications
Patients with significant central corneal scarring are not suitable candidates for CXL, as there is an increased risk of further corneal scarring.7 If a patient has a history of herpes simplex keratitis, they are at greater risk of virus reactivation and should avoid treatment for at least two years after being free of any recurrence. A dioptric difference across the cornea of more than 10 Diopters is a relative contraindication to TG-PRK because it would require too much tissue removal, increasing the likelihood of corneal haze, scarring, and regression. In very advanced cases of ectatic disease consideration should be given to a corneal transplant, which may include central corneal scarring that limits vision despite a hard contact lens, significant corneal thinning (especially less than 320 microns), or contact lens intolerance due to severe steepening.
Outcomes
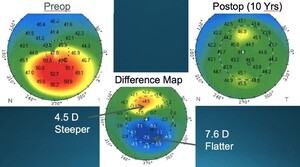
Studies have demonstrated that CXL can halt the progression of ectatic disease in 98%of eyes with a maximum corneal steepness of less than 58 D.15–18 The success rate depends on a variety of factors, including the severity of the condition, the age of the patient, and the duration of follow-up after the procedure. The use of topographic imaging can detect progressive disease by comparing preoperative and postoperative maps and calculating a difference map (Figure 13). A successful outcome will exhibit a difference map that either shows flattening in the preoperative steep areas of the cornea or demonstrates less than 1 D of steepening, which falls within the accuracy of the technology. In the rare case of progressive disease, a repeat CXL procedure may be performed if there is adequate corneal thickness. It is crucial to advise patients to avoid rubbing their eyes as it is a known cause of disease progression.
Complications
CXL, whether combined with TG-PRK or not, has been shown to be a safe procedure with low incidence of complications.19 Although complications are rare, the following postoperative conditions may occur:
-
Delayed Epithelial Healing20,21: In most cases, the epithelium becomes intact by 5 days, but a delay can increase the risk of corneal haze. Debridement of the nonhealing edge can promote epithelial migration and healing.
-
Heaped-Up Epithelium20,21: During the healing process, epithelial cells can be heaped up in a pseudodendrite-like pattern, which can affect vision if located directly over the pupil. Frequent use of preservative-free artificial tears can help with healing
-
Corneal Infiltrate20,21: A whitish infiltrate with an intact overlying epithelium is usually sterile. Rarely, it may be caused by an infection from an organism such as a fungal infection, acanthamoeba, or atypical mycobacterium. A sterile infiltrate can be differentiated from an infection by the lack of pain, minimal anterior chamber reaction, and no hypopyon.
-
Corneal Ulcer22: This is extremely rare as the UV-A light from CXL has the potential to eradicate most organisms. A white infiltrate in the presence of an epithelial defect is diagnostic of a corneal ulcer. Typically, a patient with a corneal ulcer will have pain and photophobia. Examination will show an anterior chamber reaction, and a possible hypopyon. Corneal cultures should be done in the presence of a large ulcer (>2 mm). Initial treatment is typically with a broad-spectrum antibiotic like Vigamox. In the presence of a large ulcer, it is recommended to use fortified antibiotics, such as Vancomycin and Tobramycin, that are made up at compounding pharmacy
-
Corneal Haze/Scarring23,24: Mild haze is normal and typically decreases over 4 to 6 months. Persistent haze may require a course of a topical steroid. In rare cases, the haze can be persistent with scar tissue formation. There is an increased risk of haze and/or scarring in eyes with thinner corneas, higher keratometric astigmatism, and repeat treatments.
-
Diffuse Lamellar Keratitis25: Patients with ectasia after LASIK, are at a higher risk of diffuse lamellar keratitis following CXL. These patients usually have no pain but are noted to have a cellular infiltrate in the interface below the original flap. The frequent use of topical steroids is required to resolve the inflammation.
-
Continued Long-term Flattening26: Rarely, excessive flattening can occur after CXL that is not related to corneal scarring. The pathophysiologic mechanisms that contribute to the excessive flattening are unclear. This late complication is more likely to occur in more severe disease and steeper corneas.
-
Progressive Ectasia27: Although the success rate with a single treatment is high, a small percentage of patients may require a retreatment. There is an increased risk of progressive disease in corneas with a preoperative steepness of greater than 58 D, and or those with continued eye rubbing.
Other Therapeutic or Refractive Options
Intrastromal corneal rings are another adjunct procedure with CXL to reduce irregular astigmatism and improve best-corrected acuity. Although clinical studies have shown positive outcomes in the short-term, there is a risk of long-term complications such as corneal deposits, neovascularization, and extrusion of rings. The incidence of these complications has varied in studies from 2.1%,28 6.4%,29 19.7%,30 and 30%.31 The lower incidence of complications has been seen when the femtosecond laser is used to make stromal channels versus manual dissection. These complications can be a future concern in young keratoconus patients that may live with intrastromal rings for over 50 years.
Patients who desire an improvement in uncorrected acuity may be suitable candidates for a phakic intraocular lens. Unlike corneal interventions, the use of a phakic lens does not increase the risk of ectasia. The Implantable Collamer Lens (ICL), also known as the Implantable Contact Lens, is the approved phakic lens in North America that can correct nearsightedness, farsightedness, and or astigmatism. Patients should have a satisfactory best-corrected acuity, and have an anterior chamber depth of 2.8mm or greater in myopic eyes, and 3.0mm or greater in hyperopic eyes, to qualify for the procedure.
Future Technologies
Clinical trials investigating epithelium-on CXL have generally yielded disappointing results, with an increased risk of progressive disease32. However, recent results on a new and novel technique that can achieve a high concentration of Riboflavin in the corneal stroma through an intact epithelium has shown very encouraging results,32 and is currently undergoing a final clinical study in the United States. If the positive outcomes continue, the epithelium-on method may become the preferred option for CXL, improving patient comfort, eliminating the need for a contact lens, enabling a quicker return to normal activities, and reducing the risk of corneal haze and infection.33 Additionally, if TG-PRK is necessary, it could be performed prior to epithelium-on CXL, allowing for the preservation of crosslinked tissue. This staged approach may further improve the overall results.
Early clinical studies using bioengineered corneal inlays that are crosslinked and then inserted into the corneal stroma through a pocket made with the femtosecond laser have shown an improvement in corneal regularity and best-corrected acuity (Figure 14A and 14B).34 The inlay can be folded and injected through a small incision into the stroma. Further clinical studies are required prior to gaining healthcare approval of this technology.
Corneal Allograft Rings have been reported that use human corneal tissue for implantation in stromal channels. Early reports show an improvement in best-corrected acuity and a low incidence of any complications.35 These allograft ring segments may replace traditional acrylic segments in the future.
An intraocular lens implant that is showing promise in the management of patients with irregular corneas is the pinhole implant (IC-8).36 This lens has a central clear zone surrounded by an opaque area (Figure 15A, 15B) and has received FDA approval. This lens can improve best- corrected spectacle acuity with cataract surgery or with a refractive lens exchange.
Conclusion
The utilization of CXL either independently or in conjunction with TG-PRK exhibits a considerable likelihood of achieving successful outcomes in the long-term stabilization of corneas and may also result in an improvement in best corrected visual acuity. By minimizing the need for corneal transplant surgeries, which come with prolonged healing periods and the risk of rejection, these procedures offer a valuable alternative for patients with ectatic diseases. Additionally, ongoing advancements in technology provide further optimism for the enhancement of visual quality among such patients, such as with epithelium-on CXL, bioengineered corneal inlays, corneal allograft rings, and pinhole intraocular lens implants.


._that_had_a_topography_pattern_.jpeg)












._that_had_a_topography_pattern_.jpeg)